Codeine is a narcotic analgesic most frequently used as cough relief and to treat moderate pain. Over the years, it has gained popularity when ache or pain persists even after treatment with paracetamol or NSAIDs. It has been marketed as a weak opioid and endorsed by governmental health organizations as an option to treat cancer and post-surgical pain.
Unfortunately, there has been a growing number of reports showing that weak analgesics have led to serious adverse events or even death in pediatric patients and neonates. This article will discuss the pharmacogenomics of codeine, how it works, neonatal opioid toxicity and current guidelines on the medication. Additionally, suggestions for appropriate codeine use and genomic testing prior to pregnancies are also discussed.
Codeine, Breast Milk, and Pharmacogenomics
Responses to medications are highly associated with your genetic profile and are greatly studied in pharmacogenomics to identify genetic variabilities and gene-drug dynamics. The cytochrome P450 enzyme is one of the most studied superfamilies of genes due to its association with drug adverse effects.
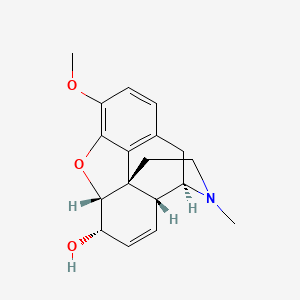
CYP2D6 is a gene from the cytochrome P450 superfamily responsible for the metabolism of many common medications, including codeine. Codeine is a weak analgesic. It is metabolized in the liver by CYP2D6 enzyme into a composition of more active metabolites. Metabolites such as morphine and codeine-6-glucuronide are mainly responsible for the analgesic effects of codeine. The extent of codeine metabolism is dependent on individual CYP2D6 genotype and hence, phenotype (poor, intermediate, normal, and ultrarapid metabolizer status), resulting in the differences in responses to codeine.
A case for neonatal toxicity was identified in April 2005 when a mother was prescribed codeine and paracetamol for 2 weeks to ease episiotomy pain after she had given birth to a healthy male infant. After 2 weeks of breastfeeding, the baby turned grey and died not long after. Postmortem analysis failed to identify any anatomical anomalies but high serum morphine concentration was detected. Concurrently, the mother’s breast milk was also highly concentrated in morphine which was later confirmed to be the cause of death of the infant. Genotype analysis for CYP2D6 revealed that the mother was heterozygous for a CYP2D6* 2A allele with a gene duplication of CYP2D6*2×2. This genotype corresponds to ultrarapid metabolizer status and is associated with significant increase in morphine formation from codeine.
Following this case, research by Madadi et al. was conducted to investigate the prevalence and mechanism of neonatal toxication by opioids. Polymorphisms in the cytochrome P450 superfamily and, to a lesser extent, UGT2B7 were the focus of the research. The authors studied genetic variants of 72 women that were prescribed codeine for obstetric pain during breastfeeding. They found two infants with mothers presenting CYP2D6 ultra-rapid metabolizer (UM) phenotype and UGT2B7*2/*2 exhibited symptoms of neonatal opioid poisoning. This aligns with the previous finding in the April 2005 case. Furthermore, the study indicated a dose-response relationship between codeine consumption and neonatal toxicity. A dose as low as 0.63 mg/kg is enough to produce signs of central nervous system depression in infants.
According to Sistonen et al., the prevalence of patients that are UM of codeine ranges between 2-40% which highlights the importance of maternal genotyping or screening prior to a prolonged period of codeine consumption.
The Current Codeine Guidelines and Genotype-Guided Prescription
Two years after the 2005 neonatal morphine toxicity case, there was a significant reduction in codeine dispensation rate for postpartum women due to the public health advisory from the US Food and Drug Admiration (FDA) supported by local clinicians. The society was informed of life-threatening pharmacogenomics-associated adverse effects and codeine guidelines were made for breastfeeding mothers.
By April 2017, the FDA published stronger restrictions for codeine prescription where breastfeeding mothers should not be prescribed codeine. If, however, codeine is required for maternal use, dosage guidelines must be followed. The lowest dose of codeine can be prescribed for no longer than four days. In the case where post-labor pain persists, an alternative analgesic will be prescribed.
In addition to strict guidelines established to minimize potential life-threatening events, genetic testing is another way to understand and avoid adverse events.
Advances in pharmacogenomics allow pre-emptive genetic screening to understand your responses to certain medications. Nalagenetics offers RxReady™, a genetic test to assess your genetic variants and aid physicians in choosing the most suitable medications. This tool analyzes the four most important genes commonly associated with adverse drug reactions including CYP2D6. Furthermore, the panel covers over 158 drugs in psychiatry, cardiology, pain management and gout management. Undertaking genetic screening with Nalagenetics could help to improve prenatal decisions in tailoring pre and postpartum medication choices.
Our suggested approach for genetic testing has been supported by researchers, regardless of its novelty in clinical practice. Recently, the US Department of Veterans Health Administration has recommended CYP2D6 genotyping to avoid issues related to opioid prescription and understand potential responses to other medications metabolized by the same enzyme.
Despite being conventionalized as a harmless cough medication, codeine has caused adverse reactions in individuals with specific genetic variants, namely those with the CYP2D6 UM phenotype. A great concern surrounds the use of codeine for postpartum pain relief. This article has discussed how mothers who are CYP2D6 UM may accidentally cause life-threatening adverse events in their infants due to the accumulation of morphine in their breast milk. Nalagenetics encourage genotyping to increase public awareness about genetic variability. Using RxReady™ could help avoid unwanted occurrences by analyzing your four genes most commonly associated with adverse effects to improve your pregnancy decision and journey. Get your genes tested now with Nalagenetics. For more information, contact 08119941440.
Leave a Reply